What is infant regurgitation?
Regurgitation means the backward movement of stomach contents up the esophagus (the “swallowing tube’) into the mouth. Regurgitation often includes the release of the material from the mouth, as in infants who “spit up.”
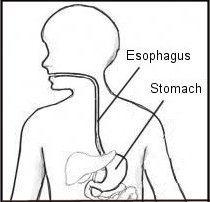
It occurs when the muscle between the esophagus and stomach relaxes (as it does during burping). This allows the stomach material up because the normal pressure within the stomach is greater than the pressure in the chest and throat.
When regurgitated stomach material comes out of the mouth, it is often mistaken for vomiting, and may look exactly like vomiting. But technically, and medically speaking, vomiting is more forceful and uncomfortable. It usually includes nausea, retching, and gagging.
Is infant regurgitation normal?
Regurgitation is a symptom that is normal and common in infants. That is because of the very small volume that the infant esophagus can hold and because of other factors, including their large liquid meals and the amount of time they spend lying down.
Infants who have a lot of regurgitation, but no actual disease, have a condition that is called functional infant regurgitation. Functional means that the symptom is real, but there is no disease. (For example, a runner’s cramp is painful but the muscle is healthy.)
Functional infant regurgitation has been defined by an international group of experts, the Pediatric Rome Working Team, as consisting of:
- at least 3 weeks of regurgitation of stomach contents,
- at least twice daily during infancy,
- the first year of life.
There must be no retching, bleeding, refusal to eat, or breathing problems, because these additional symptoms suggest a disease, rather than a functional condition. Half of all healthy infants meet these symptom-based criteria for functional regurgitation.
Should I worry if my infant regurgitates?
In the USA there are over 1 million healthcare visits yearly for infant regurgitation. Medical professionals want to help. So do formula companies and drug companies. However, the evidence that formula changes or medicines alter the course of functional infant regurgitation is generally weak.
The evidence is that no matter what you do, functional infant regurgitation gets better by itself by the end of the first year in nearly all of those who have it.
It makes no difference whether the stomach contents come out the mouth, the nose, or both. Also, the apparent forcefulness of the material coming out cannot set apart functional regurgitation from non-functional diseases.
Projectile (or forceful) vomiting occurs in some serious conditions. But projectile regurgitation that looks like vomiting is also commonly seen in functional infant regurgitation.
Signs that something more serious may be going on would include your baby having problems gaining weight, crying excessively, problems feeding, problems breathing, or throwing up blood or bile. If your child is having any of these problems you should consult your physician.
What is the difference between GER, GERD, and infant regurgitation?
It is important to know the differences between similar terms such as gastroesophageal reflux (GER), gastroesophageal reflux disease (GERD), and functional infant regurgitation.
Gastroesophageal reflux episodes occur when stomach contents move backwards up into the esophagus. Regurgitation episodes are when reflux actually reaches the mouth.
Everyone has episodes of reflux every day, but few people are aware of them. In healthy adults and infants, there is acid in the esophagus many times every day, for a total time of about one hour a day. However, reflux does not cause harm in most people, because our bodies have defenses against acid in the esophagus.
GER became a popular diagnosis only in the 1980’s, when esophageal pH testing became available. As with every new technology, there was great enthusiasm for using esophageal pH testing to measure a day-long recording of acid episodes in the esophagus. Just as a certain quantity of regurgitation episodes defines the condition of functional regurgitation, reflux episodes of certain frequencies have been used to define GER. In both of these situations, although there may be an amount of regurgitation or reflux that is greater than the average person experiences, there is no “disease.”
Gastroesophageal reflux disease (GERD) refers to tissue damage or harmful symptoms that happen because of reflux. GERD is not common in otherwise healthy infants. GERD is common following preterm birth and in infants with chronic lung disease or cerebral palsy. Common problems due to GERD include:
- Recurrent aspiration (inhaling) of refluxed material into the lungs
- Inflammation in the esophagus, causing pain, food refusal, or bleeding and anemia (low red blood cell counts)
- Failure to gain weight appropriately
Some clinicians believe that too much reflux can also cause sinusitis and ear infections. Many dentists believe that too much acid reflux into the mouth can wear away dental enamel, causing what they call dental erosions.
As noted above, functional infant regurgitation refers to regurgitation (spitting up or even what appears to be forceful “vomiting”) in a healthy infant younger than 1 year of age that occurs 2 or more times daily and lasts at least 3 weeks. By definition, there is no tissue damage or other harmful symptoms.
Functional infant regurgitation shows up as repetitive symptoms, but which have no harmful consequences. Clinicians cannot find damage to the esophagus or anywhere else in the body in healthy infants with infant regurgitation.
What tests are necessary to diagnose infant regurgitation?
No testing is necessary or desirable if your child meets symptom-based criteria for infant regurgitation.
Should I change formulas?
There is usually no reason to change formulas. The idea of changing formulas is usually because your clinician suspects protein allergy. Formula protein allergy affects 3 to 5 of 100 infants. A healthy child with spit-ups is not likely to have protein allergy. If you are formula feeding, a two-week trial of a hydrolyzed protein (hypoallergenic) formula may help any portion of the symptoms due to allergy.
What about lactose intolerance?
Lactose is the sugar in human breast milk, so babies are born with the ability to digest lactose. Lactose intolerance is rare below age 8 years, except after a severe infection of the small intestine. Lactose intolerance does not cause infant regurgitation.
What causes infant regurgitation?
Probably many factors contribute to infant regurgitation. The most important might be the size of the infant’s feeding.
The human infant must triple its birth weight in the first year. Think of how much you would have to eat next year to triple your current weight. What a wonder it is that half the healthy babies manage to keep it all down.
Adults do not notice when they have an episode of gastroesophageal reflux. They may reflux over an ounce of gastric contents, but that ounce never makes it up to the throat. That’s because the adult esophagus holds about an ounce and a half of fluid. In contrast, the infant esophagus holds only less than one-tenth of that amount. As little as a teaspoon of reflux may cause a bit of spit up in the infant’s mouth.
A reflux episode may occur every time the pressure inside the abdomen exceeds the pressure of the lower esophageal sphincter (LES). The LES is the muscle barrier that acts to prevent reflux of stomach contents into the esophagus. Increases in pressure within the abdomen are caused by routine body activities. Examples of these activities include sneezing, coughing, and bearing down to push out a bowel movement.
Treatment
Change the feeding environment
Some infants are more sensitive to their surroundings than other infants. For infants with sensitive temperaments, feedings are more likely to go well in a calm, relaxing, uninterrupted setting.
In families with lots of children (or other disruptive factors), it is best that caretaker and infant excuse themselves for 20 minutes, and go to a quiet room with dim lighting and soft, pleasant sounds.
The goal is to soothe the infant, and provide comfort. When the infant is fussy and refusing the nipple, the caretaker must remain calm, because the infant can sense the caretaker’s anxiety, and “catch” worries from the caretaker.
Thickened feeding
Several studies proved that formula thickened with cereal helps infants to nap longer, cry less, and have fewer spit ups. One tablespoon of dry rice cereal per ounce of formula is the thickener generally studied, and this thickening gives the formula 50% more calories per ounce, so the fed volume should be reduced to offset that.
Thickened feedings are especially useful if the infant’s weight is below ideal, but may be a bad idea if the infant is too heavy. Thickening formula with rice cereal may cause constipation.
Do not overfeed
With overfeeding, the infant may become uncomfortable, and learn that regurgitation will make the abdominal discomfort disappear promptly.
Drugs
Despite millions of research dollars invested by multiple drug companies to determine whether their drugs might help, no drug has been proven to reduce spitting up in infant regurgitation.
Surgery
The most common operation in the United States is the fundoplication, an operation for treating GERD.
However, fundoplication is unnecessary for functional infant regurgitation, which will resolve spontaneously by the end of the first year of life.
Effective reassurance
Infant regurgitation is a common, passing, harmless functional symptom. A clinician provides reassurance of this when listening with empathy.
Outcomes in Infant Regurgitation
As far as we know, infant regurgitation has no permanent consequences. It does not cause any problems later on in life.
Adapted from IFFGD Publication: Frequently asked questions about infant regurgitation (845) by Paul E. Hyman, MD, Louisiana State University and Children’s Hospital New Orleans, LA and Susan R. Orenstein, MD, University of Pittsburgh, PA.
